June 9, 2023 -- The National Institutes of Health (NIH) is funding work that could show how the immune system reacts to muscle disease gene therapies and lead to a protocol for re-administration of the treatments.
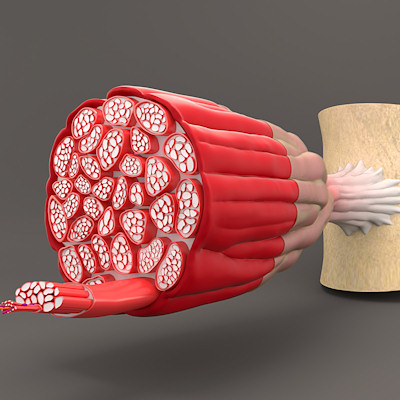
Gene therapies are emerging as new treatment options for patients with degenerative disorders such as Duchenne muscular dystrophy (DMD). The therapies could correct the cause of the genetic disorders and thereby provide lifelong benefits from a single dose. However, problems such as immune responses that limit the efficacy and duration of therapy are barriers to the realization of that vision.
Researchers at the Indiana University School of Medicine have been working on the immune problem, leading to the recent publication of a paper on concerns including antibody formation against the viral capsid, complement activation, and cytotoxic T-cell responses against capsid or transgene products.
The team has generated evidence that immune sensing drives adaptive immunity against the transgene product when patients receive muscle-directed adeno-associated viral (AAV) vector gene transfer. CD8+ T-cell responses appear to be particularly important, and the vector dose affects the roles different innate signaling pathways play in the process.
Based on the work, the researchers think steps including the engineering of vectors can minimize the immune response and increase the efficacy and duration of gene therapy. The NIH is supporting studies to advance that hypothesis through the National Institute of Allergy and Infectious Diseases.
"With our new NIH grant, we can gain a deeper understanding of how the immune system responds to these treatments so we can develop more successful and long-term ways to help patients living with muscle disorders," Roland Herzog, PhD, a professor of immunology at Indiana University, said in a statement. Herzog and his collaborators have secured a five-year, $3.8 million grant.
The description of the project submitted to the NIH, which puts the value in the first year at $774,002, lists three goals: define the mechanisms that link innate immune sensing to adaptive immune responses; prevent deleterious immune responses; and develop a novel protocol for re-administration of systemic AAV delivery.
A protocol for re-administration could transform gene therapies. Currently, biopharma companies have one chance to treat a patient's genetic disease, because when the immune system has encountered an AAV once, it is primed to attack it if it sees the vector a second time. This situation forces companies to use a high initial dose to ensure efficacy; however, that raises the risk of a harmful immune response.
Copyright © 2023 scienceboard.net