April 27, 2023 -- Australian scientists have developed a blueprint to create lab-grown human mini-lung models. The research, published Wednesday in the journal Biomaterials Research, can accelerate the development of new drugs while reducing reliance on animal testing.
Last year the U.S. passed legislation ending a requirement for new drugs to be tested on animals; Australia banned cosmetic testing on animals in 2020. Testing drugs on organoids -- 3D structures grown from human primary cells that mirror real body organs -- represents one viable alternative to animal testing for biomedical research.
Such organoids include lab-made lungs that may help address respiratory disease, the second leading cause of death globally. Given that few new lung disease therapeutics have been introduced in the last 40 years, due in part to the lack of reliable lung models, the researchers investigated lung organoids as a potential solution.
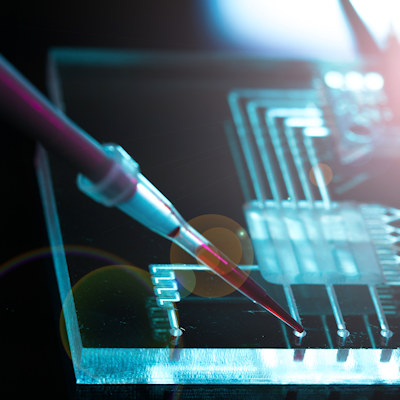
The researchers attempted to create environmental conditions for their organoids similar to those which exist in the human body, unlike traditional cell cultures grown in a Petri dish and cultured in static conditions. They began by using cells from patients, then built the organoids in layers, beginning with epithelial cells, as the organ would exist inside the body. The organoids were cultured and maintained under the micro-environmental conditions of actual lungs, with air on one side and liquid interface at the bottom, combined with microcirculation.
The researchers built two types of lung-mimicking models: healthy lungs to study the safety of new drugs; and diseased lungs that mirrored chronic obstructive pulmonary disease (COPD) to study the effectiveness of therapeutic drugs.
Because the cells come from individuals, a patient's own personalized mini-lung model can be created to test their reactions to various drugs. The organoids can also be used to test toxicity of substances, including silica dust or airborne particulates from fires. The researchers envision using these models to test the protective function of new therapeutics for high-risk patients or workers exposed to occupational hazards.
The researchers concluded that organoids can be utilized to test the safety and efficacy of new therapeutics as well as to test toxicity and injury induced by inhaled pollutants or pathogens. They say that their models' advantages include reproducibility, reliability, and cost-effectiveness on a large scale. Similar models are now being used by AstraZeneca and the U.S. Food and Drug Administration (FDA). The researchers believe organoid use can accelerate the discovery process, shorten the process of getting new drugs to clinics, and increase confidence in the molecules created before proceeding to clinical trials.
"The normal timeline for the clinical translation of a drug is about 10 to 15 years, but when you use organoid models, you can shrink that time substantially," Wojciech Chrzanowski, senior author, said in a statement. Dr. Chrzanowski, a Sydney Pharmacy School nanomedicine professor, is calling for the establishment of a national center for alternatives to animal methods to reduce the number of animals in medical research and accelerate the discovery of new drugs and innovative disease treatment strategies.
Copyright © 2023 scienceboard.net